Introduction
Obstructive sleep apnea (OSA) is a common disorder associated with snoring, upper airway collapse at sleep, oxygen desaturation and fragmented sleep. Associated with cardiovascular disease, risk of car accidents and general death. Snoring, obstructive sleep apnoea (OSA), and upper airway resistance syndrome (UARS) are conditions within the same spectrum of sleep-related breathing disorders (SRBDs).
Prevalence of OSA is 1 to 4% (adults). It affects 17% of women and 34% of men in the US and has a similar prevalence in other countries.
Definition of sleep apnea
Snoring: A noisy breathing generated from turbulence due to partial upper airway obstruction during sleep.
Apnoea: A period of no airflow at the nose or mouth for at least 10 seconds.
Sleep apnoea can be obstructive, central or mixed. In obstructive sleep apnoea, there is partial or complete airway obstruction and the patient continues to make respiratory efforts to overcome this.
Snoring and OSA in adults are more common with increasing age, in men , in the obese (body mass inde > 30), in those with a neck size of more than 17 inches and in patients with a high alcohol intake. Snoring occurs in 10% of men under 30 years and 40% of men over 60 years.
Sleep Apnea in Children
In children, it most commonly occurs around the age of 5 when adenotonsillar hypertrophy is at its greatest.
Snoring can be immensely socially disruptive and may lead to daytime sleepiness, hyperactivity and behavioral disorders.
Children's sleep apnea symptoms
Children with OSA suffer from excessive daytime somnolence, morning headaches, learning difficulties and low school performance, behavioral disorders, hyperactivity and attention deficit syndrome.
In summary: child sleep apnea signs
Nighttime: snoring, apnea, or paradoxical breathing, subcostal retractions/tracheal tugging, neck hyperextension/abnormal sleep postures, restless sleep, frequent awakenings, enuresis, parasomnias (sleep terrors, sleep walking).
Daytime: hyperactivity, sleepiness, poor school performance, neurocognitive deficits, behavior problems (anxiety, aggression, depression, somatization), unrefreshing sleep/difficulty waking in the morning, mouth-breathing/dental or craniofacial changes, dysphagia.
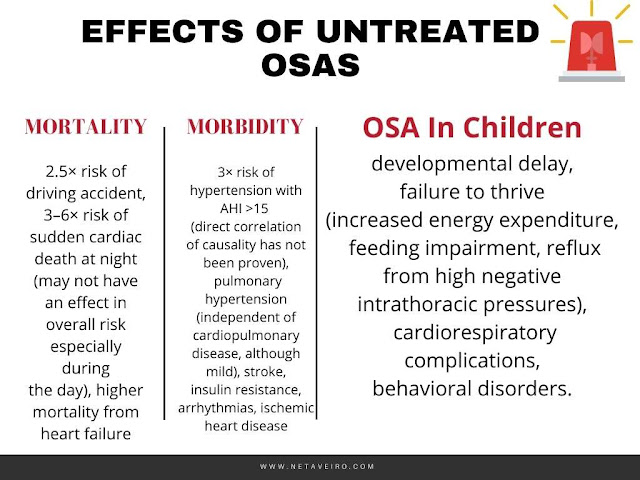
OSA Complications: developmental delay, failure to thrive (increased energy expenditure, feeding impairment, reflux from high negative intrathoracic pressures), cardiorespiratory complications, behavioral disorders.
When should I be worried about sleep apnea?
- Snoring (up to 95%)
- Witnessed apnoeas
- Nocturnal arousals or arousals with sensation of “choking”
- Excessive daytime sleepiness
- Morning headaches
- Reduced libido
- Mood changes
- Poor concentration ◦
- Reduced quality of life
- Impact on daily activities, e.g., driving
Can I self diagnose sleep apnea? Try This home sleep apnea test
Epworth sleepiness scale This is a self-scoring questionnaire to identify those who may have OSA and therefore should have a sleep study.
These 8 situations are described and for each situation the patients must score themselves according to their chance of dozing.
The situations are described below:
- Sitting reading a book.
- Watching television.
- Sitting inactive in a public place, for example, a meeting or theatre.
- Lying down to rest in the afternoon when circumstances permit.
- Sitting talking to someone.
- Sitting quietly after lunch without alcohol.
- In a car, stopped in traffic or at traffic lights.
- h. In a car, as a passenger for an hour.
The situations are scored as below:
- 0 Would never doze.
- 1 Slight chance of dozing.
- 2 Moderate chance of dozing.
- 3 High chance of dozing.
Interpretation of total score/24 is as follows:
- 0–5 Low normal daytime sleepiness.
- 6–10 High normal daytime sleepiness.
- 11–12 Mild excessive daytime sleepiness.
- 13–15 Moderate excessive daytime sleepiness.
- 16–24 Severe excessive daytime sleepiness.
Sleep apnea risks factors you should know about
- Raised body mass index (BMI)
- Increased neck circumference
- Retrognathia/micrognathia
- Macroglossia
- Increasing age
- Tonsillar hypertrophy
- Large soft palate or uvula
- Sedative and alcohol use
- Floppy eyelid syndrome
Sleep Apnea Treatment Options
Snoring and OSA are often multi-factorial conditions with a variety of primary causative factors, hence there will never be a single treatment to cure snoring.
Accurate assessment is essential and will guide treatment. Weight loss to reduce BMI to the normal weight range (< 25) may reduce neck size and tongue base bulk.
Exercise helps to increase palatal and pharyngeal muscle tone which in turn helps to prevent airway collapse in the presence of negative pharyngeal pressure. In the early evening, exercise promotes restfulness too.
Good sleep hygiene All patients with sleep-related breathing disorder will benefit from practising good sleep hygiene.
This means getting into good habits and practices and creating the correct environment for a better-quality sleep.
Personal habits
- Establish a regular bedtime routine, getting to bed and rising at similar times each day.
- Regular exercise reduces stress, anxiety and depression.
- Avoid vigorous exercise too close to bedtime; late afternoon exercise can cause somnolence a few hours later when the body has recovered and cooled, allowing sleep to come more readily.
- Eating healthily and not too close to bedtime.
- Avoid caffeine, nicotine and alcohol close to bedtime (within 4 hours ideally) as these may act as stimulants.
- Our circadian rhythm is triggered by light and darkness, so try to be outdoors for periods during the day and evening and have minimal light when sleeping.
- Some find relaxation techniques such as yoga or meditating help to relax the mind and promote restfulness.
Sleep environment
- Associate the bedroom with sleep. Do not watch television or look at electronic devices.
- Keep the bedroom dark so as not to disrupt one’s circadian rhythm, quiet and cool.
- Have a comfortable bed.
What is the newest treatment for sleep apnea?
There are several therapeutic options, consult your doctor.
References:
Guidelines for Diagnosing and Treating Sleep related Breathing Disorders in Adults and Children