1. Clinical Definition
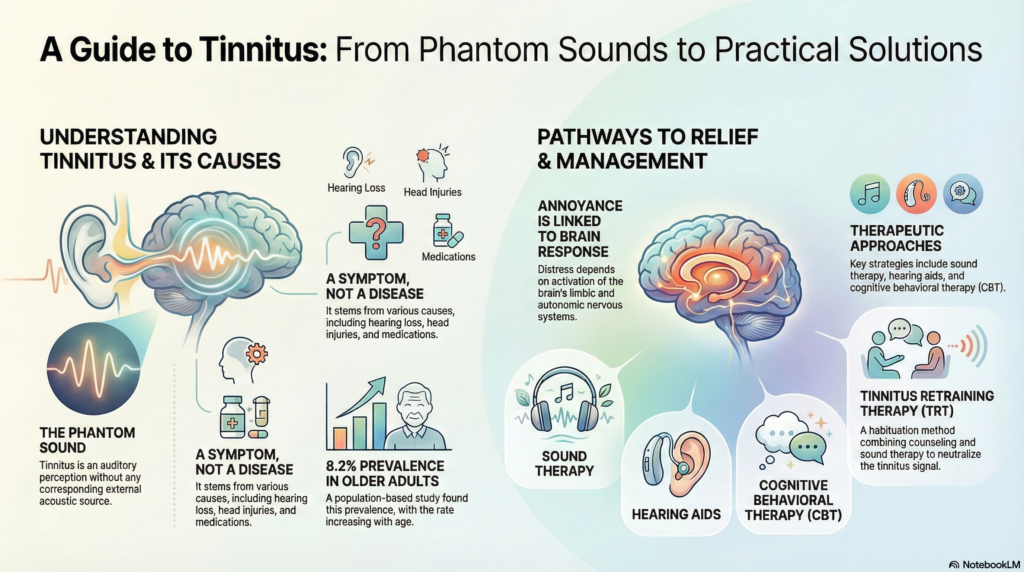
Tinnitus is the registration of sound in the central auditory cortex without mechanical vibration in the cochlea (subjective type). It represents a failure of the “gating” mechanisms in the auditory pathway. Clinicians must distinguish this from auditory hallucinations; tinnitus is a simple phantom percept (ringing, buzzing), whereas hallucinations involve complex patterns (voices, music).
2. Mechanistic Analysis: The Somatic Connection
The majority of tinnitus cases arise from central crosstalk. Specifically, the Dorsal Cochlear Nucleus (DCN) receives both auditory and somatosensory inputs. When auditory input is diminished (hearing loss), somatosensory signals from the jaw or neck are amplified via ephaptic coupling.
(Noise Trauma / Hearing Loss)
(Brain increases sensitivity)
(Dorsal Cochlear Nucleus Activation)
(Limbic System Engagement)
3. Applied Clinical Approach
To accurately diagnose the etiology, apply the tri-phasic Dr. Belh Framework:
Phase 1: Observation
Analyze the “Auditory Library”. Low-frequency “roars” suggest Meniere’s. High-pitched “cicadas” suggest sensorineural loss. Pulsatile sounds indicate vascular origin.
Phase 2: Context
Assess Somatic Modulation. Does jaw clenching, neck rotation, or eye movement alter the pitch/volume? Confirm central crosstalk mechanism.
Phase 3: Classification
Isolate the category. Differentiate Subjective (neural, only patient hears) from Objective (mechanical, observer hears). Rule out “Red Flags” like acoustic neuromas.
4. Extraction Zone (Key Points)
- The 10dB Rule: In subjective tinnitus, the perceived intensity is rarely more than 10dB above the hearing threshold, yet distress is high due to limbic involvement.
- Threshold Phenomenon: Onset is often cumulative; noise exposure + stress + fatigue trigger the perception.
- Adaptation vs. Habituation: Adaptation is a peripheral sensory function (ear); Habituation is a central processing function (brain).
- Somatic Tinnitus: A specialized subtype where physical movement (bruxism, neck pressure) modulates frequency or volume.
- Ototoxicity: Salicylates, NSAIDs, and Aminoglycosides are primary pharmacological triggers.
5. Synthesis Table: Subjective vs. Objective
| Feature | Subjective Tinnitus | Objective Tinnitus |
|---|---|---|
| Audibility | Patient only (Internal) | Patient + Observer (Stethoscope) |
| Primary Origin | Neural (Auditory Cortex/DCN) | Vascular (Blood flow) or Mechanical |
| Associated Pathology | Hearing loss, Noise trauma, Meniere’s | Carotid stenosis, Palatal myoclonus |
| Clinical Insight | Common Habituation possible | Rare Treatable surgically |
6. Natural Course & Timeline
The progression of tinnitus follows a distinct temporal pattern. While the auditory signal may become permanent, the psychological distress typically diminishes.
High Distress
Established
Neutral Signal
7. Visual Reference Prompt
8. Frequently Asked Questions
Is tinnitus a disease?
No. Tinnitus is a symptom of an underlying condition, such as hearing loss, Meniere’s disease, or vascular issues.
Can stress cause tinnitus?
Stress acts as a modulator rather than a root cause. It activates the limbic system, making the perception of existing tinnitus louder and more intrusive.
Is it permanent?
If symptoms persist beyond two years, the condition is clinically classified as permanent. However, perception often decreases via habituation.
What is the “roaring” sound?
A low-frequency roar (125-250 Hz) is a specific hallmark of active Meniere’s disease, often accompanied by vertigo.
Does aspirin cause tinnitus?
Yes, high-dose salicylates are ototoxic and can trigger reversible tinnitus. Paradoxically, aspirin can abolish tinnitus caused by spontaneous otoacoustic emissions.