Translational Tinnitus Solutions: A Strategic Clinical Roadmap
Clinical Abstract: Audiology is pivoting from theoretical observation to translational “bench-to-bedside” application. Current subjective measurement models create insurance barriers and stall capital investment. This roadmap outlines the transition to objective biomarkers, device-led therapy, and genetic precision medicine to validate tinnitus as a treatable pathology.
Translational Research in Audiology
Translational research is the systematic process of converting basic scientific discoveries into immediate clinical applications (“bench-to-bedside”). In the context of tinnitus, this represents a fundamental departure from long-term, observational studies toward high-velocity, device-driven interventions.
The current clinical landscape is characterized by a “learning to live with it” philosophy. The strategic imperative is to replace this with active resolution protocols. This shift requires moving from low-capital theoretical grants to high-capital (“McLaren-level”) funding structures capable of supporting complex device engineering and large-scale genetic sequencing.
Mechanistic Analysis: The Funding-Outcome Cycle
The stagnation in tinnitus cures is mechanistically linked to the lack of objective proof. Without biological verification, reimbursement fails, choking upstream investment.
1. Objective Biomarker Identification
2. Insurance Parity & Reimbursement
3. High-Capital Investment Flow
4. Clinical Resolution
Applied Approach: The Dr. Belh Framework
To implement this roadmap, we apply a tripartite structure focusing on the current deficit, the context of failure, and the necessary clinical solution.
1. Observation
Subjective Liability: Current diagnostics rely on patient self-reporting (TFI scores). This introduces emotional bias and prevents standardization.
2. Context
The Gray Area: Insurers do not reimburse pathologies they cannot measure. Lack of a “blood test” equivalent creates a financial bottleneck.
3. Solution
Objective Verification: Development of EEG signatures and genetic panels (108 genes) to establish tinnitus as a measurable biological fault.
Key Clinical Milestones
- Establishment of Objective Biomarkers: Moving beyond the Tinnitus Functional Index (TFI) to EEG data and Otoacoustic Emissions (OAE) signals.
- Device-Led Neuromodulation: Focus on Bimodal and Multimodal stimulation. Research must define specific “Efficacy Windows” to determine optimal intervention timing (early vs. late stage).
- Genetic Subtyping: Screening for the 108 identified genes linked to tinnitus severity, allowing for preventative intervention before cognitive decline occurs.
- AI Integration: Utilizing Artificial Intelligence to categorize global clinical datasets and identify neural signatures invisible to human analysis.
Transition: Subjective vs. Objective Measures
The following table illustrates the required shift in clinical diagnostics to achieve the strategic roadmap.
| Category | Current Standard (Subjective) | Future Standard (Objective) |
|---|---|---|
| Methodology | Patient reporting & psychological scales | Data-driven Neurological signatures |
| Diagnostic Tools | TFI, VAS (1-10 Scale), Pitch Matching | EEG Analysis, ABR Testing |
| Reliability | Variable (Influenced by mood) | Constant (Biological reality) |
| Outcome | Measures perceived distress | Identifies physiological pathology |
Strategic Implementation Timeline
The progression from current research to global standardization involves distinct phases of technological maturation.
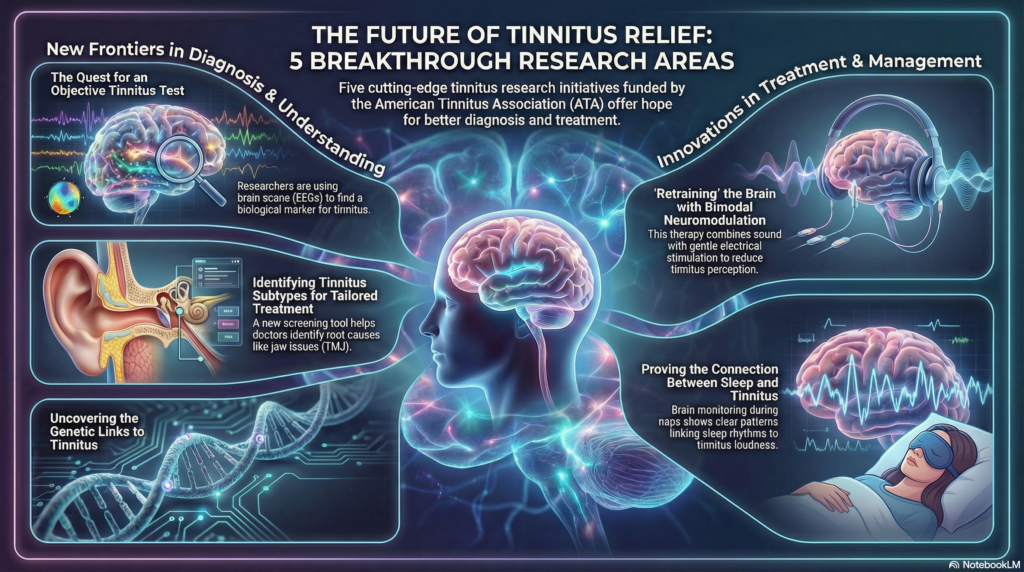
2025 Tinnitus Research: Breakthroughs in Treatment and Diagnostics
Clinical FAQ
1. Why is objective data crucial for tinnitus treatment?
Objective data (biomarkers) is necessary to validate the physical presence of tinnitus, enabling insurance reimbursement and attracting high-level research investment.
2. What is the role of genetics in this roadmap?
Researchers have identified 108 genes linked to severe tinnitus. Screening for these allows for differential diagnosis and early preventative care.
3. How does neuromodulation differ from hearing aids?
Hearing aids amplify sound. Neuromodulation (bimodal/multimodal) actively stimulates the auditory system and brain to retrain neural pathways.
4. What is the “Efficacy Window”?
It is the hypothesis that treatments may be significantly more effective if applied during a specific timeframe (acute vs. chronic) after symptom onset.
5. When is the TRRI conference?
The Tinnitus Research Initiative (TRI) conference is scheduled for 2027 in the United States, serving as a milestone for global research alignment.